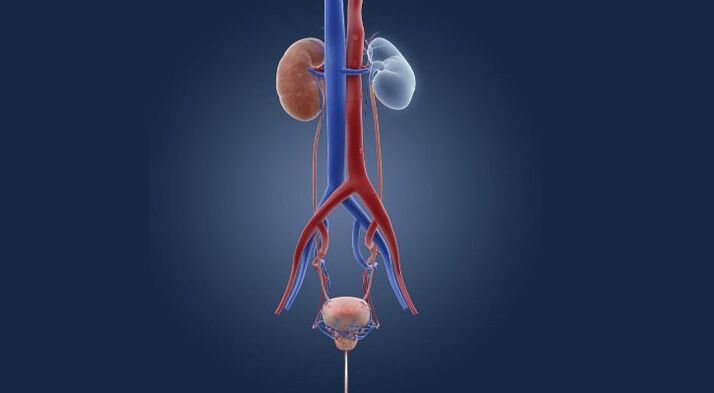
Cystitis is inflammation of the bladder. This organ is intended for the accumulation and excretion of urine, but if the organ's lining is damaged, its function suffers and the person begins to experience unpleasant symptoms. In most cases, the pathology affects only the mucous membrane, but sometimes the inflammatory process also extends to the muscle tissue. Interstitial cystitis is the most difficult to deal with.
The disease mainly affects women, which is associated with the anatomical features of the urethra. Inflammation in men appears rarely, it usually acts as a comorbidity against the background of chronic prostatitis.
Symptoms
The signs of cystitis are quite obvious and it is difficult to miss them. As a rule, the disease begins acutely, which is why patients pay attention to the obvious discomfort in the urinary tract. Among the manifestations of known pathology:
- frequent need to urinate;
- feeling of incomplete urination;
- cramps and pain when urinating;
- increase in body temperature;
- the appearance of a mixture of blood in the urine;
- cloudy urine (due to the presence of pus);
- nausea, drawing pains such as during menstruation.
Despite the characteristic symptoms, the disease can have different manifestations. Hematuria is not always present, but the intensity of the pain may only resemble mild discomfort. In any case, if signs of pathology appear, it is necessary to consult a doctor to make a diagnosis as soon as possible. The disease in the acute phase at an early stage is better treated, but the chronic form takes longer to fight.
Forms and types of chronic cystitis
By the nature of the inflammatory process, cystitis is acute and chronic. Depending on the source of development, the disease can be primary (an independent disease) or secondary (inflammation spreads from adjacent areas, such as the kidney).
According to the area of damage to the mucous membrane of the bladder, cystitis occurs:
- total (general);
- focal.
The following clinical forms of cystitis are distinguished:
- catarrhal - non-purulent inflammation of the bladder mucosa;
- phlegmon - purulent lesion of the submucosal layer;
- granulomatous - accompanied by rashes on the mucous membrane;
- hemorrhagic, which is characterized by the release of blood in the urine;
- interstitial cystitis - inflammation spreads to all layers of the organ.
Numerous rare forms are also distinguished: ulcerative, cystic, gangrenous cystitis.
The whole variety of inflammatory diseases of the bladder is combined into two large groups:
- specific cystitis, which are caused by pathogens of sexual infections: gonococci, ureaplasm, chlamydia.
- Nonspecific cystitis - develops due to the fault of opportunistic flora, the representatives of which under normal conditions do not lead to diseases (for example, E. coli).
Finally, non-infectious cystitis is combined into a separate group. They can occur under the influence of allergic factors, radiation, traumatic, thermal effects, parasite toxins.
Causes of cystitis

In most cases, damage to the bladder and the development of the inflammatory process are associated with the penetration of infection, however, cystitis can be toxic and allergic in nature. When an infection occurs, the disease is transmitted in several ways:
- ascending - from the urethra through the urethra - affects the bladder;
- descending - in this case, the infection appears due to inflammation of the kidneys, through the ureters, reaches the bladder;
- lymphogen - from the flow of lymph through the pelvic organs in the presence of lesions of the genital organs;
- hematogenous - infection enters the bloodstream, but this route of spread is the rarest;
- direct - if an abscess ruptures inside the bladder and pathogenic microflora penetrates directly into the bladder cavity, it can also be during catheterization of an organ, an infection during surgery.
Most often, E. coli causes cystitis. It occurs in 80-95% of cases of simple pathology. This bacterium is normally found in the rectum, but when it enters the urethra it causes an inflammatory process. Enterobacteria, staphylococci, fungi, sexually transmitted infections can also cause the disease. It usually precedes the onset of symptoms of vaginitis or bacterial vaginosis, and you may also notice symptoms of the disease within a day of sexual intercourse (postcoital cystitis).
Factors contributing to the development of cystitis
The body with good immunity can cope with the presence of pathogenic microflora, so the symptoms of cystitis in the patient will not appear. But when exposed to some factors, it manifests itself:
- injury to the mucous membrane of the bladder;
- circulatory disorders of the pelvic organs;
- hypothermia;
- the presence of other foci in the body, such as kidney infections;
- decrease in the body's defenses;
- inflammatory diseases of the genital organs;
- lack of vitamins and minerals in the body;
- hormonal imbalance;
- insufficient hygiene, wearing synthetic underwear;
- stress and overwork;
- delayed emptying of the bladder.
In the presence of these factors, cystitis will progress rapidly and the chronic pathology will pass to the stage of relapse. Therefore, in order to prevent relapses, it is necessary to exclude the influence of provoking factors on the body.
Causes of the transition of acute inflammation to the chronic stage
The inflammatory process in the bladder can occur due to various pathogens. Most often these are bacteria, but there are cystitis and viral and fungal etiology. If the acute form of the disease is diagnosed in time, the correct treatment of cystitis is prescribed, and the patient follows all the recommendations of the doctor, then the pathological process can be completely eliminated and recovery will come.
But often women postpone visits to the doctor, try to cure cystitis on their own, hoping that everything will go away on its own. As a result, valuable time is lost. Microorganisms actively multiply, the intensity of inflammation increases. Having fully "settled" in the bladder, the microbes will not give up their positions so easily. The inflammation becomes chronic.
It is also common for a specialist to prescribe a treatment for cystitis, the patient starts taking medications, and stops the therapy on her own when she feels relieved. As a result, the pathogens are not completely destroyed, and the survivors divide - chronic cystitis is formed, which is resistant to antibiotic therapy.
Finally, the following circumstances contribute to the development of chronic cystitis:
- general decrease in immune defense, hypothermia;
- hormonal changes (pregnancy, menopause);
- neglect of the rules of personal hygiene;
- gynecological diseases;
- chronic diseases of other organs and systems: diabetes mellitus, malignant tumors.
Signs of chronic cystitis
In today's medical community, the term "chronic cystitis" itself is obsolete. It is used "the old way", for better communication with patients. A slow inflammatory process in the bladder is called recurrent cystitis. Its main symptom is the development of 2 or more exacerbations within six months or 3 episodes per year.
The period of exacerbation is accompanied by characteristic symptoms:
- frequent urination;
- pain, burning, pain when urinating;
- night calls;
- feeling of incomplete emptying, pain in the lower abdomen.
Exacerbation of the disease may be accompanied by a moderate increase in body temperature, the appearance of blood in the urine, its turbidity.
During the period of remission, symptoms can be completely alleviated. But more often than not, patients suffer from discomfort when urinating and moderate periodic pain for years.
The most serious consequence of recurrent cystitis is the development of resistance (resistance) of pathogens to antibacterial drugs and the subsequent degeneration of the bladder mucosa. The mucous epithelium undergoes scar deformation or is replaced by a stratified squamous one. At this stage, chronic cystitis can no longer be cured with antibiotic therapy alone. It is necessary to carry out special medical procedures.
Acute and chronic cystitis: therapeutic approaches
Treatment of acute and chronic forms of pathology is different. Usually, acute cystitis is much easier to treat, because the pathology is provoked by microorganisms, against which the doctor will prescribe a course of antibiotic therapy. Antibacterial drugs are quite different. They quickly help to stop an attack of the disease, and the systematic use of funds will lead to a complete cure for cystitis. Preparations based on fosfomycin perfectly cope with inflammation.
Chronic inflammation is more difficult to treat because it is complicated by other ailments. Complex treatment of long-term developing cystitis is carried out using several groups of drugs. Antibiotics remain in the lead, but the doctor will also prescribe anti-inflammatory drugs, vitamins and reparants. As a prevention of infections and to consolidate the effect of therapy, the patient is prescribed herbal remedies, physiotherapy courses.
cystitis in women
Most often, cystitis in women is accompanied by exacerbations of chronic inflammation, therefore, according to statistics, every second patient consults a doctor with a recurrent disease twice a year.
This speaks not so much about the difficulties in treating the disease, but about the need for careful observance of the doctor's prescriptions and the elimination of the factors that provoke the disease.
cystitis after intercourse
Postcoital cystitis in women is caused by genitourinary abnormalities. When it is moved down and into the external opening of the urethra, it becomes more susceptible to the penetration of pathogenic microflora. Also, the culprit of postcoital cystitis is an overly mobile urethra, which moves easily when the penis is rubbed. In this case, the mucous membrane is easily irritated and pathogenic microorganisms penetrate the opening of the urethra. Symptoms and treatment of this form of pathology are interrelated, so doctors approach the problem individually in each clinical case.
In addition, the causes of cystitis are the alternation of anal sex with vaginal sex, which is absolutely impossible, because the microflora of the rectum enters directly into the vagina and the adjacent urethra. A factor in the development of bacterial infections is the manual introduction of microbes, insufficient secretion of vaginal mucus, which causes microcracks.
Symptoms of postcoital inflammation do not differ, but the patient can notice their appearance directly in connection with sexual intercourse - usually discomfort occurs already in the first 12 hours.
Treatment of postcoital cystitis is individual, since it is first necessary to determine the cause of the disease and accurately direct therapy. With an abnormality of the urethra, the doctor will suggest plastic surgery, as a result of which the problem will disappear. Both surgery and hyaluronic acid injections are possible. If an STI infection occurred during an intimate relationship, antibacterial drugs will be needed, followed by restoration of the vaginal microflora.
What does the blood in the urine say
The appearance of blood in the urine indicates the development of acute hemorrhagic cystitis. It does not appear at the end, but it accompanies the entire urination process. The presence of erythrocytes gives the urine a pink color. In addition, the urine may be the color of "meat slops", that is, have a brownish color with the presence of brown threads, threads or flakes of mucus.
Usually, when you urinate with blood, there is severe pain, pain in the bladder and pulling sensations in the lower back. The appearance of blood in the urine is a mandatory reason to consult a doctor.
Cystitis during menstruation
In some women, an exacerbation of cystitis occurs against the background of hormonal changes during menstruation. During menstruation, the pelvic organs are more susceptible to infections, so the following can provoke the disease:
- inflammatory diseases of the female genital organs;
- hormonal fluctuations;
- allergic reaction to intimate hygiene products;
- decrease in the body's defenses;
- failure to comply with personal hygiene;
- non-specific infections, mycoses, sexually transmitted diseases.
Under the influence of these factors, the pathogen enters the urethra and urethra, causing inflammation. Usually, an exacerbation of the disease occurs during ovulation, as well as 1-2 days before the onset of menstruation. Vaginal discharge becomes an excellent breeding ground for pathogenic microflora. Symptoms of cystitis during menstruation are typical, but they are complicated by characteristic manifestations during menstruation: aching and pulling pains in the lower abdomen.
The doctor can identify the cause of the pathology after taking a medical history and studying the results of laboratory diagnostics. The treatment regimen is standard, but simultaneous treatment of gynecological pathologies may be required if genital infections are diagnosed. It is important to observe personal hygiene, strengthen the immune system.
Pregnancy and cystitis

According to the results of studies, doctors found that asymptomatic bacteriuria is detected even before pregnancy, so it is during the gestation period that the disease manifests itself. The reasons for this are:
- changes in the hormonal background and in the ratio of progesterone to estrogen in the body of the expectant mother;
- violations of urodynamics with increasing size of the uterus;
- weakening of the ligament apparatus, increased mobility of the organ, but a decrease in its peristalsis and tone;
- expansion of the renal pelvis due to increased blood circulation in the pelvis.
The latent course of the disease complicates early diagnosis. Treatment of cystitis during pregnancy is also possible with the use of antibiotics. The doctor will prescribe drug names and drug dosages that are safe for the fetus.
Diagnostic methods
Symptoms of cystitis are very characteristic, but the doctor will still prescribe a series of tests to finally find out the causative agent of the pathology and determine the nature of the course of the disease. The specialist will collect an anamnesis, analyze the patient's complaints and conduct an external examination with palpation of the bladder area. The following diagnostic methods are used:
- ecoscopy - using ultrasound, it is possible to determine the degree of the inflammatory process, its prevalence and assess the condition of the urinary system, genital organs;
- cystoscopy - examination of the organ using an endoscope, which allows you to assess the condition of the bladder mucosa;
- cystography: an examination of the bladder using a contrast agent.
In women, treatment should begin with the definition of the pathogen. A series of laboratory tests is mandatory: general urinalysis, Nechiporenko analysis, bacteriological culture, tissue biopsy, polymerase chain reaction (for a more accurate determination of the pathogen). To assess the degree of the inflammatory process, doctors can send a blood test. If inflammatory pathologies of the female genital organs are suspected, an examination by a gynecologist and the delivery of the examinations prescribed by him may be necessary.
Methods of treatment
In inflammatory diseases of the organ, doctors resort to therapeutic and surgical methods for the treatment of pathology. In most cases, it is possible to eliminate the disease with properly formulated drug therapy with the addition of physiotherapy.
Drug treatment includes a combination of several effective drug groups, depending on the nature of the disease. The patient can be given:
- anti-inflammatory drugs - serve to relieve swelling of the mucous membrane and eliminate pain, the inflammatory process is reduced;
- antispasmodics - used to relieve pain symptoms, effectively eliminate bladder spasms;
- antibacterial therapy - a group of drugs that act directly on the causative agent of the pathology;
- antifungal drugs - recommended if cystitis is provoked by a fungus or complicated by it (for example, with a combined course of a bacterial-fungal infection);
- phytopreparations - medicines in tablets and other forms that have antimicrobial and anti-inflammatory properties.
In some cases, doctors prescribe drug instillations to the patient instead of oral administration. Washing of the bladder is done in the clinic. With the help of a special catheter, the desired concentration of the drug is administered, which cannot be achieved in other ways. Before the procedure, the patient must empty himself so that the drug affects the mucosa for as long as possible.
Surgical treatment is used only in rare cases, when the inflammatory process has provoked anatomical changes or in severe recurrent infections. In this case, laser correction is performed. For example, in postcoital cystitis, for many women, the only treatment option is distal urethral transposition.
Diet in the treatment of cystitis

It is imperative to follow a diet, as spicy and salty foods contribute to the appearance of ulcers on the mucous membrane. Other products are irritants that interfere with recovery:
- foods rich in sugar;
- citrus, acidic, fermented foods;
- seasonings;
- tomatoes and all dishes with tomato, additives (ketchup, sauces, adjika);
- soy sauce and vinegar;
- nuts and chocolate.
To accelerate healing, the patient is advised to eat a light and nutritious diet. It is necessary to exclude fried foods, smoked meats, marinades, fatty foods. It is best to steam, stew or boil. Eliminate all foods that can trigger allergies.
An attack of cystitis can also be provoked by heavy food, in which the patient suffers from constipation. With stagnation of fecal masses, intestinal peristalsis worsens, stagnation occurs in the bladder, as a result of which the mucous membrane is again irritated. It is because of the high protein content that you shouldn't eat too much meat, fish, beans, cheeses. Replace them with foods rich in fiber: vegetables and fruits allowed.
During the treatment, try to eat at home, cooked and not include new foods or dishes on the menu. Keep in mind that the diet completely excludes alcoholic beverages and also limits coffee and tea. Juices, infusions and decoctions of herbs, fruit drinks and compotes will be useful. It is best to replace regular water with slightly alkaline mineral water.
Physiotherapy
Among the methods of treating the disease, physiotherapy is widely used. As a rule, it is recommended in the healing phase, when acute inflammation of the bladder has been removed and a positive trend towards healing has occurred. Physiotherapy is also effective for the submucosal localization of the causative agent of the pathology, when antibacterial drugs do not have the correct effect. Since physiotherapy is used:
- phonophoresis;
- electrophoresis;
- magnetotherapy;
- UHF;
- modulated currents.
The session does not last long, however, a course of 10-15 procedures is required to achieve the effect. Powerful treatment of cystitis in combined ways will help to completely get rid of the disease.
Question Answer
How long does cystitis last?
The duration of cystitis depends on the form of the pathology. The acute one lasts 7-10 days, after which, with proper treatment, recovery occurs, but the chronic form of the disease can last several months, remembering periods of exacerbation.
Is it possible to visit a hot bath or shower with cystitis?
A hot shower or bath really helps to relieve spasm and pain, however, these thermal effects are contraindicated in inflammation of the bladder, as this contributes to the aggravation of the inflammatory process.
Which doctor to contact and which tests to deliver?
Women with suspected cystitis should contact a general practitioner, men - a urologist. If necessary, the patient can be referred for examination by a gynecologist. Tests - urinalysis, blood work, and ultrasound or cystoscopy.
How does age affect the course of the disease?
Most often, cystitis occurs in women between the ages of 20 and 45, which is associated with active sexual activity, unstable hormone levels and an increased risk of developing gynecological pathologies. In older women, the condition occurs less frequently and is associated with a weakened immune system.
Is it possible to cure chronic cystitis?
Like any other chronic disease, cystitis manifests itself with periods of exacerbation and remission. It is difficult to completely cure the disease, but with the right treatment it is possible to achieve a stable and very long remission without any symptoms from the urinary system.
Do I need a special diet for the signs of cystitis?
Yes, during the period of exacerbation of the disease, patients are advised to follow a diet with the exception of salty, spicy and irritating foods. Despite the presence of frequent urination, you should not strictly limit yourself to fluid intake. You can drink up to 2 liters of pure water, compote, weak tea. But alcohol and coffee in the acute stage are prohibited.
What characteristics should be considered when choosing a uroseptic?
Let's start with the fact that the selection of the drug and the appointment of an antibiotic regimen is a task only for a specialist: a urologist, a nephrologist, a therapist. It is unacceptable to stop the treatment of cystitis yourself or to change the remedy.
The use of tetracyclines, cephalosporins in cystitis quickly leads to resistance of pathogens. Therefore, drugs from these groups are practically not used for the treatment of cystitis. Doctors prescribe ampicillin, fluoroquinolones and various combinations of uroseptic agents. Herbal uroseptics are also widely used, the main advantage of which is good tolerability and almost complete absence of contraindications. Preparations of this group can be used to treat pregnant and lactating mothers.
The doctor selects a uroseptic individually, analyzing the data of each clinical case. To determine the sensitivity of pathogens to a particular antibiotic, a special study is performed - a bacteriological analysis of urine with inoculation on nutrient media.
How to treat cystitis yourself at home and can it be done?
If symptoms of cystitis appear, it is necessary to consult a urologist, nephrologist or general practitioner as soon as possible. Only a specialist can correctly assess the features of the clinical picture, conduct a comprehensive examination, make a correct diagnosis and prescribe the necessary treatment.
But often patients are faced with the fact that the doctor's appointment is scheduled for a certain time and the pain must be relieved at this time. To reduce the rate of progression of the pathological process, observe the drinking regimen: drink about 2 liters of water, compotes, fruit drinks. Hypothermia is a common cause of aggravation of the condition, so it pays to dress warmly and protect yourself from drafts.
Also try to avoid overexertion. Rest (physical and sexual) will help to wait for an appointment with a specialist. It is undesirable to take analgesics and antispasmodics alone without extreme necessity: they can "lubricate" the clinical manifestations of the disease and it will be more difficult for the doctor to make a correct diagnosis.




























